Whether it’s a grand religious affair under a vaulted cathedral ceiling in Salisbury or under the branches of an oak tree in a Wolverhampton burial ground, people want to say ‘words’ as a last goodbye, as a last thank you. For an elderly person this should be a celebration of their life: it’s sad, but you know it’s the order of things.
You’re giving the eulogy to the audience, wherever you happen to be – and one last word to your parent/friend/relative/partner.
The audience is people who knew them, family friends, neighbours, fellow club members, but generally friends all.
To celebrate the person, you want to celebrate the life, so you can use that as the skeleton for the eulogy – tell the life story, tell people what they did, where they were when they were five, twenty five, forty five. What was life like for them back then? Was it wartime, post wartime?
Brainstorm ideas, gather all the key points and individual personal events from friends and family, ask for stories – they’ll be happy to be included in the process.
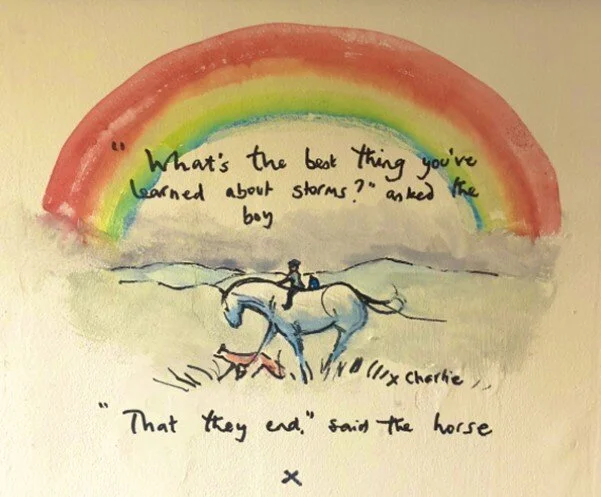
Read other eulogies and don’t be afraid to borrow lines that resonate with you, and that would have fitted in with the lost relative.
Introduce yourself and the other direct family members – the neighbours might not know who you are, and often they’ll want to speak to the family after with tales of memories and their loss.
Write out the eulogy longhand on paper; it’s a cathartic process and helps you to organise your memories and at the same to wash through the emotional pain involved with death of a close person. You’ll want to speak through the eulogy, and not be overcome (these notes came from groups of folk in America, they work).
A timeline is a great way of organising what you say – it automatically brings in places they lived, times and events they knew, places they went to school/university, places they worked, homes they had, holidays they took, and skills/hobbies/sports that threaded through their life. As you go through the timeline those events will resonate with the folk in the audience and bind them into the celebration.
The best eulogies have lots of stories, and relevant humour: that’s the way we tend to remember our nearest & dearest, we remember the happy times and the laughs.
Check the time allotted – it’s not a lecture, there’s more to tell about some than others, in general keeping towards 10/15 minutes or so should not upset the vicar!
Dealing with the emotion: if it’s a close parent/relative then even its after their 105th birthday the finality is upsetting. We’re human, we get upset and we cry when we’re very upset – it’s tough to deliver a eulogy when you’re stumbling with tears so here’s the exercise that’s tried and tested: the day or morning before, after you’ve written out the eulogy take it to the bottom of the garden, the loft, a locked bathroom, and read it out, deliver it to the tree/mirror/door in front of you. Read it through verbatim. When you’ve finished reading it out, start again. The American chums suggest reading it out loud six times – we agree. It flushes through the emotional stress, gets you all cried out so you can deliver a brilliant clear, fluent eulogy of celebration of which your Mum/Dad/Gran would have been proud.
No one ever teaches you how to write a eulogy, and generally you can’t ask your parents by the time you need to, so here are some examples to give you inspiration.
Steve Job’s eulogy by his sister.